The impact of OA
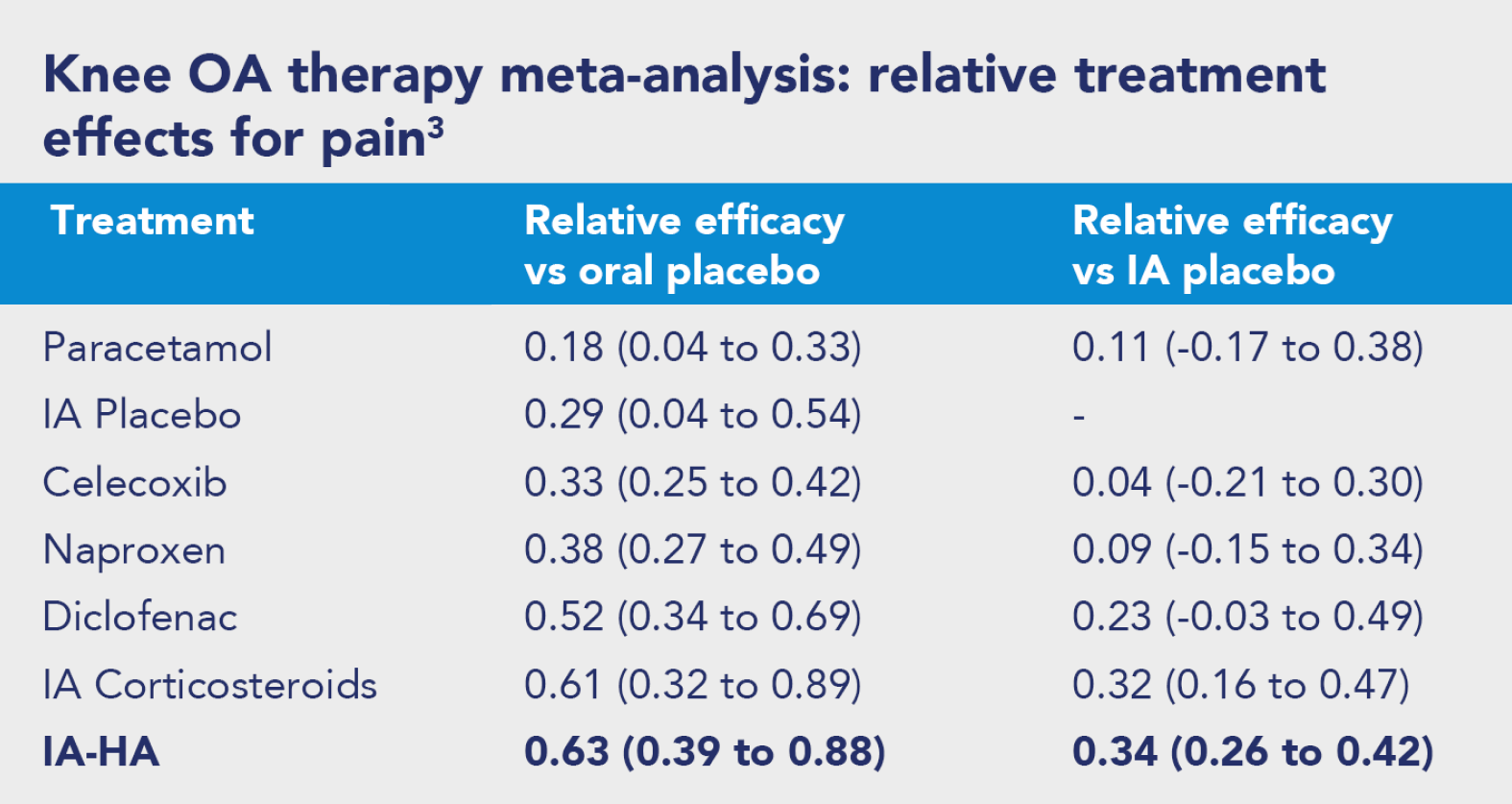
OA can lead to chronic pain. Pain is a multi-factorial experience, influenced by biological (degree of OA in the joint), psychological (thoughts and feelings about their OA) and social factors (not being able to exercise or work due to OA). Everyone will have unique factors influencing their pain, therefore it is essential a person- centered approach is adopted to improve pain, function and quality of life.